
Advancing Orthopedic Care
The Transformation of Bone Grafting through Advanced and Innovative Approaches. "Employment of a 3-D cylindrical osteotome for autogenous bone grafting is engineered for the 360° extraction of iliac crest bone grafts; these are solid living bone tissues. This 3-D tool possesses extensive applications in the field of orthopedic surgery. The ease of acquiring ICBG with this device expands the utilization of bone-grafting procedures in patients who medically require such interventions."

For Orthopedic Surgeons
Spine, Plastic, and Oral Surgeons
VIDEO DEMO: https://www.youtube.com/watch?v=caQHtFe19Qs
Discover the World's First and Only "3-D" Tricortical Graft Harvester System.
NOW YOU CAN CAPTURE THE GOLD STANDARD AUTOGRAFT WITH CONFIDENCE, CONVENIENCE AND EASE, WITH 'TEMPLATED HARVESTING TECHNIQUE' .
Harvest the cancellous, unicortical, bicortical, and tricortical bone grafts
FDA CLASS I EXEMPT PRODUCT Request Your Sample Today : Contact Dr. Kelly
This is not an ordinary trephine bone harvester, but rather the world's first and uniquely designed model with the most extensive capacities. It is equipped with integrated tricortical curette-cutters, specifically for the purpose of minimally invasive trephining and large volume bone harvesting. The device is engineered to extract the tricortical graft by the simple activation of a button, detaching the bone core effortlessly. It is now available in various large diameter sizes, ranging from 12mm, 14mm to 20mm, 23mm, or 25mm, and in selective lengths. This innovative technology is positioned to significantly reduce time, energy, and effort in the workplace. The internal cut-out and readiness for use are additional features that distinguish this product.

Consider the potential that this faculty of the trephined curettage technique presents; it is boundless.
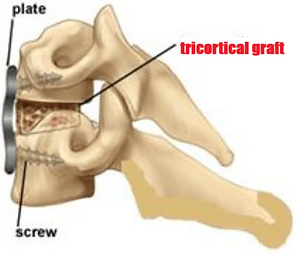
ACDF:
Smith Robinson tricortical graft technique.
Given that the typical width of the pelvic rim is about
20mm-25mm

A Plunge is all that is Required, Followed by a Complete 360° Capture and Rapid Procurement.
"FAST AND SAFE, ONE-SHOT-DONE !"

Research and Development at
Barrow Neurological Institute, USA
Our Goal: To Promote Trephinated Curettage Technique and To Expand the Scope to Enhance The Overall Success of Spinal Fusion Surgeries. Furthermore, once realized, this approach offers the lowest cost of care for the global healthcare systems, for the long term, in view of rising costs and aging population. Autograft remains the most commonly implemented graft method to this day. Each alternative option comes with its advantages and drawbacks, but an important consideration when treating patients is the cost of care. This is paramount.
EXPLORUS SURGICAL is dedicated to revolutionizing bone grafting procedures with innovative solutions that advance orthopedic care. Our team is committed to developing cutting-edge technologies that enhance patient outcomes and redefine surgical practices. This instrument is like a surgical explorer designed to MIS harvest ICBG, including the autograft iliac crest tricortical graft, the "C-Shape Graft", and this is revolutionary.

Driven by a passion for rendering the lowest risks of complications overall and improving orthopedic procedures, our team of experts works tirelessly to create safer, more efficient solutions that set new standards in the industry.
"In an ideal world, you can harvest any bone you need just by using the trephine, and all it takes is to take a bite to take out the bone, to Keep It Simple and Safe, the "KISS rule."
The color-coded marking lines are not aligned at the beginning of the bone harvesting process, but at the end of the procedure when no more resistance is felt the color-coded marking lines are aligned. This confirms and indicates that the bone harvesting process is completed and the device containing the cancellous or tricortical bone graft can be gently removed with ease and without resistance.
Our Mission

Research and Development at
Barrow Neurological Institute, USA
Bone grafting is a widely used form of tissue transplantation, second only to blood transfusion. The rising incidence of bone and joint disorders along with a rapidly growing geriatric population are fueling the demand for orthopedic surgeries that use bone grafts.
Autograft – Patient’s own bone tissue, also known as autologous bone, is considered the “gold standard” of bone-grafting material. Autogenous bone is the only graft material that fulfils all three components of the tissue regeneration triad: osteogenesis, osteoinduction, and osteoconduction. It is also biocompatible, which means that bone harvested from the patient’s own body has no risk of rejection or disease transfer. Autologous bone naturally contains viable cells such as osteoprogenitor cells, as well as essential molecular components like bone morphogenetic proteins (BMPs). Furthermore, autologous bone can provide a calcium scaffold required to support the new bone growth. Autologous bone can be harvested as a tricortical graft for structural support.
At EXPLORUS SURGICAL, our mission is to provide healthcare providers with advanced bone grafting solutions that enable them to achieve superior patient outcomes and optimize surgical procedures.
Innovation
We are dedicated to constant innovation, ensuring that healthcare providers have access to the latest advancements in bone grafting technology to deliver exceptional patient care and improve surgical efficiency.
Impact
We are committed to making a significant impact on the orthopedic industry by offering innovative bone grafting solutions that enhance patient care outcomes and streamline surgical procedures.
Commitment
Our team is committed to developing state-of-the-art bone grafting solutions that empower healthcare providers to deliver superior orthopedic care and achieve excellence in surgical procedures.
INTRODUCTION



Worldwide, there are millions of patients each year suffering from bone-related illness due to trauma, degenerative diseases, infections or oncology that require orthopaedic intervention involving bone grafts. Bone autografts, iliac crest bone graft ICBG remain the gold standard since there are no issues with histocompatibility or disease transmission while possessing the ideal characteristics: osteogenicity, osteoconductivity and osteoinductivity.
INNOVATIONS
The trephination technique is a well-known bone marrow biopsy method that has been used for diagnostic purposes. Later, the same technique was modified and described as a bone graft harvesting method by enlarging the trephine diameter, and has been used for many years. The trephination technique has become popular because it can be performed in a smaller incision, and fewer complications have been reported compared to the conventional curettage technique. However, the volume of obtained graft is important for most orthopedic procedures, especially if the size of the bone defect is large. Importantly, autogenous bone grafting is a powerful tool because it can offer the surgeon ample cortical or cancellous bone to achieve osseous union.
The criteria for the trephine technique is to always allow for the harvest of an adequate volume of cancellous bone and ideally also cortical bone, including cortico-cancellous bone grafts.
This innovative minimally invasive bone harvester is specially designed and engineered to help you consistently deliver optimal patient outcomes by further enlarging the trephine diameter to optimally increase the internal capacity that allows you to harvest adequate volumes of cortical and cancellous bone; including cancellous, unicortical, bicortical, and tricortical grafts, unlike traditional methods, unlike conventional curettage, and unlike all the ordinary trephines. This is extraordinary.
This is a user-friendly device, the harvest procedure is completed in 3 minutes, and easy to learn; a short learning curve and pickup.

WITH ONE QUICK-HARVEST, THIS IS ALREADY ONE-SHOT-DONE LIKE A "HOLE-IN-ONE."
In this way; simply by using a 12mm (14mm,or 16mm) D x 20 mm L trephine, even one
single-pass can already harvest adequate amounts of ICBG cancellous bone for 1-level ACDF spinal fusion in instances when interbody cage in conjunction with spinal instrumentation are used; the cage can be packed with an adequate 12mm (14mm, or 16mm) D x 20mm L cancellous bone providing immediate stability to the anterior spinal column and a favorable environment for fusion.
On the other hand; simply by using a 20mm (23mm, or 25mm) D x 15mm L trephine, even
one single-pass can already harvest an ample ICBG tricortical graft for 1-level ACDF spinal fusion, without the need for using any Ti/PEEK
artifical interbody cage.

AUTOGRAFT HARVESTING SYSTEM


Autograft Harvesting System
Autograft Harvesting System is a patented bone harvesting surgical instrument set and registered with the FDA, for uses in a variety of medical surgeries including spine, orthopedics, trauma, foot-and-ankle, plastic, dental, oral and maxillofacial surgeries. The instrument set enables a minimally invasive approach to harvesting autogenous bone and can offer the capability to safely cut and to rapidly harvest the solid living autogenous bone graft tissue from the iliac crest in a bone harvesting system. Furthermore, Autograft Harvesting System facilitates and enables the surgeon to perform a Closed Osteotomy Technique in the process of rapidly harvesting the solid living autogenous bone graft tissue from the iliac crest to provide all the essential osteogenic, osteoinductive, and osteoconductive properties required to achieve a solid osseous union and bone fusion.
IMPACT

With this systematic trephinated curettage technique approach, the trephine is now combined with internal curettes to harvest bone cores synergistically, this functions perfectly well to harvest all relevant grafts, including the cancellous, unicortical, bicortical, and tricortical grafts. This is a heads-up and offers new advantages relating to reducing admission time, post‐operative analgesia requirements and donor site complications, whilst also reducing incision length and shortening operating time compared with other techniques to impact usage significantly.
When used appropriately, and with practice experience, the actual total bone procurement procedure for harvesting the tricortical graft takes less than 3 minutes.



Overall, surgeons performing multilevel ACDF use a nonstructural component and the most common nonstructural component is autograft iliac crest cancellous. Autograft tricortical iliac crest graft was most often chosen as the gold standard for choice of graft material for ACDF. The “gold standard” most often chosen by surgeons was autograft iliac crest tricortical bone.
To avoid associated problems of graft harvesting, synthetic cages are an alternative, but cannot provide biological fusion. As for synthetic cages, the major issue with Ti alloys is its low bone-bonding ability; thus, increased research has been done on surface chemical and physical and morphology modifications to improve bone bonding.
PEEK provides stability similar to that of Ti alloys, and in some cases improves durability, strength and overall biomechanical profile. PEEK has radiographic properties that allow surgeons to better monitor possible migration and the success of the implant. However, the primary issue with PEEK is that it is hydrophobic and unable to sufficiently bond to bone to achieve solid fusion. This may be associated with cage migration and pseudarthrosis (nonunion). Polyetheretherketone (PEEK) cages have been widely used in patients with degenerative disorders of the cervical spine. Their radiolucency and low elastic modulus make them attractive attributes for spinal fusion compared with titanium. Still, limitations are seen such as pseudoarthrosis, subsidence, and migration of the cages. The major disadvantage of PEEK as an implant is its biological inertia, which results in poor bone binding ability and weak antibacterial performance after implantation, thereby seriously hindering its clinical application to a large extent. In particular, the poor bone integration of PEEK implants induces the formation of fibrous wrapping, which may lead to implant failure and nonunion.
Clinically, cage constructs were associated with “both lower and slower fusion rates”. Furthermore, the cages were associated with device fragmentation and erosion (pistoning) into the adjacent vertebrae (more severe than simply subsidence). Thus it appears that ACDF with a dynamic plate and autograft was superior to cages for
anterior cervical fusion.
PHILOSOPHY
Autograft ICBG remains the gold standard of all bone grafts. The bone graft plays the pivotal role in promoting bone healing. The minimally invasive ICBG harvester is designed to harvest ample cortical and cancellous bone to achieve osseous union, and helps you consistently deliver optimal patient outcomes. Harvest ICBG autologous cortical and cancellous bone quicker, easier, and safer.
Although enormous efforts have been made in bone regeneration therapy, autologous bone grafting is still a necessary and frequently used procedure. Although utilization of allograft, synthetic materials, and demineralized bone matrix (DBM) has increased, autologous bone graft is still considered “gold standard” as it contains all properties necessary to generate bone; autologous bone graft is osteoinductive, osteoconductive, and osteogenic. Because autologous bone is harvested from the patient, it is nonimmunogenic, histocompatible, and does not transmit diseases. ICBG remains the gold standard of all bone grafts, and can be harvested as a corticocancellous or cancellous bone graft.
In common with the trend in other surgical specialties, minimally invasive methods of iliac crest bone harvesting have been tried in order to reduce morbidity and enhance the overall success of spinal fusion. These include the use of a curette, bone biopsy needles and trephines. Therefore, the improvement of bone graft harvesting approaches, and the development of bone graft substitutes emerge as fundamental components of future research endeavours to enhance the success of spinal fusion surgeries.
Despite intensive research and development of potential bone graft alternatives, autologous bone graft remains the gold standard of care for treatment of bone defects. The union rate associated with autograft bone appears greater than with alternative bone grafts. The major impetus for the development of bone graft substitutes was to mitigate the complications associated with the harvest of autologous bone. For the foreseeable future, for most nonunions, autograft bone remains the gold standard.
Overall, autograft is considered superior to allograft because of its excellent and cost-effective combination of biologic and mechanical properties. Autologous bone grafts continue to be an important tool in the management of certain bone defects or nonunions. In one study comparing bone graft treatment in 182 patients with long-bone nonunion, the autograft populations showed a significantly shorter union time with fewer surgical revisions and significantly lower postoperative infection rates. Immunological reactions from an allograft may interfere with the process and can lead to graft rejection. Additionally, they carry the added risk of transmitting bacterial and viral diseases. Limitations center around the risk of disease transfer, decreased mechanical strength, and poor osteogenic abilities. Another important consideration when using allografts is the antigenicity of the bone. Studies that have compared the integration of allograft bone with that of autograft bone have demonstrated slow integration of the allograft cohort with incomplete vascularization and decreased osteoinduction and osteoconduction. Studies noted the inferiority of allograft bone material in cervical fusion compared with autografts and surgeons tend to preferentially choose autografts over allografts for spinal fusion.
Epstein cited 100% fusion rate for 60 patients undergoing 1-level ACDF utilizing iliac autograft and dynamic plates
(ABC; Aesculap, Tuttlingen, Germany). Fusion occurred an average of 3.8 months [range 2.5-8 mos] postoperatively.
Riew, Heller, Sasso, et al., presented (Cervical Spine Research Society, Phoenix, AZ, unpublished) a post-hoc analysis of their data obtained from a prospective, randomized, multicenter study originally designed to compare cervical disc arthroplasty with 1-level ACDF (allograft/plates). They discovered a much lower initial fusion rate for the single-level allograft/plated fusions than had previously been reported. The fusion rate was only 55.7% at 1 year, while it gradually increased to 92.3% at 4 years. The evidence showed much lower 1-year fusion rates of only 55.7% for allograft/plated
1-ACDF then had previously been reported. For this low fusion rate, the surgeons should have reevaluated their use of allograft for the l-level ACDF constructs as the patients require more time to fusion.
Unfortunately, most synthetic bone graft substitutes lack appropriate osteoinduction, osteoconduction, and osteogenicity. Some show potential, like BMP-2 (Bone Morphogenetic Protein-2) but were also associated with potential serious complications including ectopic bone formation and possible cancer risks. The fusion rates with alternative bone graft substitutes like BMP-2 is still unclear and fusion rates range widely between studies. Several studies investigated the complication spectrum of BMP-2, including carcinogenicity, and reported a wide range of potential complications, complication rates, and controversial conclusions. Ultimately, incorporation of BMP-2 results in fusion rates approaching, but still potentially inferior to, those seen with autograft alone. Additionally, retrospective studies have not established an association with improved fusion rates following BMP use, adding doubt regarding the necessity of its application. To avoid associated problems of graft harvesting, synthetic cages are an alternative, but cannot provide biological fusion.
DIAMOND CONCEPT
Alternatives to autologous bone grafts lacks one or more of the concepts of the ‘‘Diamond Concept’’ of Giannoudis: osteogenic cells and vascularization, mechanical stability, growth factors, osteoconductive scaffolds (in combination with growth factors), that are a prerequisite for bone healing. Moreover, most alternatives are expensive and not validated by Evidence Based Medicine (EBM), thus being scarcely recommendable for clinical use.
TRADITIONAL ILIAC CREST BONE GRAFT HARVESTING TECHNIQUES

This diagram shows the difference between (A) corticocancellous, and (B) cancellous iliac crest bone graft. Unicortical (1A) and bicortical (2A) bone grafts are obtained through subcrestal windows; unicortical bone grafts are typically harvested from the outer table of the ilium and bicortical grafts include the inner and outer table of the ilium. Tricortical (3A) grafts are obtained from the iliac crest at least 3 centimeters posterior to the anterior superior iliac spine (ASIS).
TREPHINATED CURETTAGE TECHNIQUE
Bone graft extraction using a trephine to fill a trephine tube will remove a core of cancellous bone graft. This method has also been grouped under 'minimally invasive' ICBG harvest by many authors. There is evidence that the trephine method reduces admission time, post‐operative analgesia requirements and donor site morbidity, whilst also reducing incision length and shortening operating time compared with open techniques.
Once with using the enlarged trephine diameters fully-equipped with the end-cutters to cut the back-end of the graft, this newly creates the proper and effective "TREPHINATED CURETTAGE TECHNIQUE" and offers new advantages, to standardize and systemize bone harvesting, and with a potential viewpoint to replace all of the above diverse traditional harvesting techniques with the purpose to reduce the complications related to the donor area. The innovative concept is that the trephine component will plunge-cut down into the pelvis and create an initial bone core, followed in-sequence by the internal forceps to address the base of the bone core to detach it from the native ilium bone, and inadvertently serves as a curette to procure the entire bone core securely out of the ilium. With this complete formality in place, thereafter, all relevant structural bone grafts can be harvested in this systematic fashion.
The trephine method (trephination) is a proper ‘Closed Surgery’ ICBG harvest; this is a Minimally Invasive Method for harvesting autograft iliac crest cancellous and cortico-cancellous bone, including the ‘tricortical graft'. Since the trephination technique is performed in a blinded fashion, the three-dimensional structure of the ilium should be kept in mind, and the depth of the trephination should be controlled. The likelihood of complications can occur and increase when heavy pressure is applied, rather than gently allowing the delicate instrument to do its own work. Do not apply heavy pressure on the device at all times. This entire process is essentially passive and not aggressive. High-speed and incremental consistent light forces will negotiate into the pelvic bone most effectively. Follow the instructions. To prevent cortical penetration, the trephine should be positioned and advanced following the pelvic anatomy. Another issue to be considered to prevent iliac bone perforation is the adjustment of the trephine depth to stay less than 30mm, or better still, to stay within 20mm depth. Also to note is that the average width of the adult pelvic rim is typically 20mm-25mm wide. Both the direction and the depth of the trephination are of utmost importance for a safe trephination technique.


TRADITIONAL TRAPDOOR TECHNIQUE



Trapdoor methods involve any procedure where a bone flap (or 'trapdoor') is made in the iliac crest from which subcortical bone graft is removed before the flap is replaced to restore the cortical anatomy. This method is 'open', as the cortex is intentionally split to access cancellous bone.
The trapdoor technique is used to longitudinally split the medial and lateral edges of the iliac crest, expose the cancellous bone between the medial and lateral plates, preserve the inner plate, and a gouge harvests the cancellous bone of the iliac crest. It has been suggested that trapdoor methods are associated with a greater admission time and analgesia requirement compared with closed methods (e.g. trephination) for ICBG.
Therefore it might be more beneficial to the patients to maximize the use of trephination; by using a 12mm (14mm, or16mm) D x 20mm L trephine can harvest adequate bone volumes required, and/or even with using multiple-passes to obtain relevant larger amounts could already avoid the cortex to be intentionally split to access cancellous bone. In all events, the trephination closed method is always preferable.
The problem of donor site morbidity after the harvesting of autologous bone grafts may be reduced by modified or improved harvesting techniques or the use of other donor sites. The greater trochanter of the femur is mainly composed of cancellous bone that is suitable for use in surgery. The greater trochanter of the femur is another useful autogenous bone source and free bone graft can also be obtained by using this trephine device. A 12mm D x 20mm L can obtain useful cancellous bone volumes from the greater trochanter of the femur. In the same fashion a 12mm D x 30mm L trephine device can obtain useful cancellous bone volumes from the femoral medullary canal.
GRAFT CONCEPT IDEAS
It is widely acknowledged that iliac crest autograft serves as the gold standard, given its essential properties of being osteoconductive, osteoinductive, and osteogenic. An ideal bone graft should possess all these attributes concurrently.
Despite the significant advancements in the manufacture of synthetic bone substitute materials, autograft bone graft continues to be the gold standard, as it fulfills all the necessary criteria. Furthermore, autograft bone graft does not pose a risk of disease transmission, does not elicit immunogenic reactions, and possesses exceptional regenerative and remodeling capabilities.
A subsequent surgical intervention at a remote donor site may potentially give rise to several complications, including, but not limited to, chronic pain, hematoma and seroma formation, iatrogenic fracture, neurovascular injuries, abdominal hernia, and infection. It is worth noting that graft donor site pain is extensively documented as the most prevalent donor site morbidity. The prevalence of autograft site pain has prompted numerous companies to develop a multitude of bone graft substitutes, albeit with limited evidence of efficacy.
At present, the anterior iliac crest remains the most frequently utilized donor site in orthopedic surgery, enabling the procurement of a substantial quantity of bone graft. The anterior iliac crest bone graft may be obtained using various techniques, resulting in the harvesting of cortical, cancellous, or corticocancellous bone grafts.
Structural Grafting in ACDF
Corticocancellous grafts can be classified as unicortical, bicortical, or tricortical, and offer the significant advantage of supplying immediate structural support. These grafts can be initially incorporated utilizing a press-fit technique or internal fixation through various methods, which subsequently impact its immediate strength. The strength of cancellous and corticocancellous grafts enhances as bone mass accumulates and remodelling occurs.
The procurement of cancellous bone graft from the iliac crest is executed through a corticotomy with a surgical burr or osteotome, ensuring the preservation of the inner and outer tables of the cortical iliac bone. Subsequently, the graft is extracted utilizing curettes, hand gouges, or rongeurs. It is imperative to meticulously adhere to the ilium's path to circumvent fractures.
The trap-door technique for the iliac crest involves the longitudinal splitting of the medial and lateral edges of the iliac crest, unveiling the cancellous bone between the medial and lateral plates, while preserving the inner plate, and ultimately procuring the cancellous bone.
Employing alternative harvest techniques, such as trephinated curettage, facilitates reduced soft tissue dissection and has been suggested to diminish postoperative pain associated with graft harvest.
Unicortical and bicortical bone grafts are usually obtained through the application of a subcrestal window technique, which involves the stripping of musculature from both the inner and outer table of the ilium. Traditionally, unicortical bone grafts are sourced from the outer table of the ilium, with due care taken not to breach the inner table. Bicortical bone grafts encompass both the inner and outer table of the ilium. Tricortical and bicortical grafts are frequently utilized in anterior interbody spinal fusion surgery, as the additional cortex provides significant structural integrity. Tricortical bone grafts comprise the inner and outer iliac tables as well as the iliac crest.
The inclusion of multiple cortices in graft structure bolsters its structural integrity. However, the implications and consequences of soft tissue stripping must not be disregarded. In a study conducted by Chen et al., the efficacy of inner-table only and inner-outer table exposure techniques for anterior tricortical bone graft harvest in pediatric patients was compared. The results indicated that exposure of solely the inner table of the ilium facilitated faster healing of the donor-site defect. This limited exposure preserves the periosteum and the vascularity of the superior gluteal artery, thereby expediting the healing process at the donor site.
Conversely, exposure of both the inner and outer tables of the ilium could significantly compromise the cosmetic appearance due to the lower healing potential at the harvest site. Furthermore, extensive soft tissue stripping could potentially expose patients to an increased risk of infection, wound healing complications, and pain. As such, soft tissue stripping should be minimized to the greatest extent possible.
TREPHINATED CURETTAGE TECHNIQUE – A NEW APPROACH
Given that the typical width of the pelvic rim is commonly 20mm-23mm.
A. Unicortical Grafting for ACDF Cloward Technique
The most basic method involves utilizing a 12mm Diameter x 20mm Length Trephine Bone Harvester Device. This tool facilitates the direct extraction of a Unicortical Bone Graft, identical in size, from the top of the iliac crest. This approach completely avoids the stripping of soft tissue from both the inner and outer tables of the ilium, thus maintaining their integrity.
Unicortical Graft ACDF Cloward Dowel Technique
12mm (14mm,16mm) Diameter x 20mm Length
For ACDF Cloward Technique
This can be supplemented by a press-fit technique plus internal fixation for instrumented graft fusion using plate and screws, or even double-plating, subsequently enhances its immediate strength, to simulate a bicortical graft, and to resume an equivalent multiple cortices status.
Plate and Screws Fixation
* The benefits of acquiring Unicortical bone grafts (plugs) with diameters of 12mm, 14mm, or 16mm and lengths of 20mm include, at a minimum, a broad surface of contact, ensuring a graft/vertebral end plate interface of 1 cm x 1 cm. Additionally, it concurrently addresses the necessity of adequate graft height to satisfy the spine space requirement.
This Unicortical grafting approach is unique and exclusive, and cannot be accomplished by using a miniature 3.5mm trephine, which cannot provide adequate graft height to fulfill the spine space.
*Cancellous bone regeneration and restoration of the local anatomy of the ilium are possible after intracortical bone harvesting. This regeneration of the iliac cancellous bone permits re-harvesting within as little time as 24 months to provide autologous bone graft to assist fusion in subsequent operations.
Ref: Spontaneous Posterior Iliac Crest Regeneration Enabling Second Bone Graft Harvest; A Case Report
Elias C. Papadopoulos, MD Patrick F. O’Leary, MD Ioannis P. Pappou, MD Federico P. Girardi, MD Hospital for Special Surgery 2009 HSS Jrnl (2009) 5: 114–116
B. Bicortical Grafting for ACDF Smith-Robinson Technique
The most straightforward method of bicortical grafting is achieved through the use of a Trephine Bone Harvester Device with a diameter of 20mm and a length of 15mm. This instrument facilitates the direct acquisition of a substantial bicortical bone graft from the iliac crest's top, including only the inner table. By exposing solely the inner table of the ilium, this approach facilitates quicker healing of the donor site defect and completely eliminates the need for soft tissue stripping from the outer table of the ilium.
Bicortical Graft (inner table only) ACDF Smith-Robinson Technique
20mm Diameter x 15mm Length
For ACDF Smith-Robinson Technique.
The bicortical graft obtained in this way is of sufficient size that it could be chiseled down
to fit into a cervical disc space as in the Smith-Robinson ACDF technique, and fixated with plate and screws.
This can be supplemented by a press-fit technique plus plating, internal fixation for instrumented graft fusion using plate and screws, or even double-plating reinforces its immediate strength, to simulate a tricortical graft, and to resume the equivalent multiple cortices status.
The maximization of the contact surface area between fusion surfaces was first advocated for by Cloward as a means to promote bony fusion. Cloward proposed that an optimal bone fusion surface area encompassed 80% of the intervertebral endplate's surface area. However, this advice is often disregarded nowadays, leading to many unsuccessful surgeries. Cloward recommended that 80% of the end plate should be covered by intervening interbody bone graft. Unfortunately, this is seldom achieved in current times.
Whilst the surgeon may be apprehensive about subsidence due to the load being concentrated on a minimal surface area of contact, the crux of the matter is that the surface is not minimal; rather, it is expansive. In both of these scenarios, there is typically a 1 cm x 1 cm graft/vertebral end plate interface, at the very least. This is the reason for its superior efficacy compared to all other methods. That is why this is significantly more successful than the other strategies.
However, it necessitates meticulous attention to detail, as the surgeon must procure the iliac graft and skilfully modify it to ensure a precise press-fit, unlike the procedures for cadaver allograft and PEEK CAGE systems, which may allow for a more cursory approach. In these ideal grafting methods, we must depend on the surgeon's expertise in graft placement, combined with the dynamic plate, which enables the graft to remain securely in place and ultimately fuse, and it stays in and fuses, as demonstrated on 3-month postoperative CT scans.
C. Tricortical Grafting for ACDF Smith-Robinson Technique
The most straightforward method of tricortical grafting is achieved through the use of a Trephine Bone Harvester Device with a diameter of 20mm and a length of 15mm. This instrument facilitates the rapid 360°direct acquisition of a substantial tricortical bone graft from the iliac crest's top via minimal dissection. This technique is performed in a blinded fashion thus the three-dimensional structure of the ilium should be kept in mind, and the depth of the trephination should be controlled.
Tricortical Graft ACDF Smith-Robinson Technique








Meet Our Experts
Our diverse team of experts brings a wealth of experience and dedication to every project. Meet the leaders driving our mission to revolutionize bone grafting procedures forward.

Surgeons

Research Scientists

Biomedical Engineers
Product Development Team
What Surgeons Say
EXPLORUS SURGICAL's innovative bone autografting solutions transforms orthopedic procedures for improving patient outcomes to enhance the overall success of spinal fusion surgeries.
“We were impressed with the ease and time of the overall procedure. It all went smoothly overall. The detachment of the tricortical graft felt perfectly smooth in fact I was surprised I was already all the way though as it took less than 20 seconds. The curettage was very sharp, clean and even. We were impressed with the ease with which the tricortical harvest procedure went in such a short time period and it was of sufficient size to fit into a cervical disc space.”
"This device is useful and successful for harvesting bone grafts. It has some important advantages, such as ensuring a more quick harvest when compared to the traditional method.
The bone core comes out in a cylindrical shape that can be directly used as graft for ACDF anterior cervical spine discectomy and fusion. The iliac bone is an ideal site for use of this device and the cores seems to be in good shape when it is used in a ACDF cervical fusions. The availability of different sizes of this devices could allow bone graft harvests for different procedures such as posterior facet distraction and fusion, and anterior and posterior lumbar fusions."
Dr. Brian P. Kelly Ph.D.
Dr. Anna G.U.S Newcomb M.S.
Dr. Jennifer Lehrman M.S.
Dr. Bernardo de Andrada-Pereira M.D.
Researched and Developed at;
Dignity Health,
St. Joseph’s Hospital and Medical Center,
Barrow Neurological Institute,
350 West Thomas Road, Phoenix,
AZ 85013, USA.




"I highly recommend EXPLORUS SURGICAL for their groundbreaking autografting solutions, and to raise awareness. Training is important." Dr. Brian P. Kelly Ph.D.
References
-
C.E. Gillman and A.C. Jayasuriya Materials Science & Engineering C 130 (2021) 112466 Department of Orthopaedic Surgery, College of Medicine and Life Sciences, University of Toledo, 3000 Arlington Avenue, Toledo, OH 43614, USA. Elsevier B.V. (2021).
-
A. Cakar, O.F. Egerci, F. Dogruoz et al. Comparison of curettage vs. trephination technique for harvesting anterior iliac crest bone graft: A cadaveric study Department of Orthopedics and Traumatology, Istanbul Training and Research Hospital, Istanbul, Turkey. Chinese Journal of Traumatology (2023).
-
Clinical guidelines for indications, techniques, and complications of autogenous bone grafting. Chinese Medical Journal 2024;137(1).
-
Kakalecik et al., Iliac Crest Bone Graft: A Review. JOrthoBusiness.org | January 2025, Vol 5, No 1Department of Orthopaedic Surgery & Sports Medicine, University of Florida, Gainesville, FL. College of Medicine, University of Florida, Gainesville, FL, USA.
-
Stewart SK, Fracture Non-Union: A Review of Clinical Challenges and Future Research Needs. Malaysian Orthopaedic Journal 2019 Vol 13 No 2.
-
Letchuman et al., Bone grafting and biologics for spinal fusion in the pediatric population: current understanding and future Perspective. Neurosurg Focus Volume 50 • June 2021.
-
Advances in implants and bone graft types for lumbar spinal fusion surgery. Biomater. Sci., 2024, 12, 4875–4902 | 4875.
-
Demetriades et al. What Is the Evidence Surrounding the Cost-Effectiveness of Osteobiologic Use in ACDF Surgery? A Systematic Review of the Literature. Global Spine Journal 2024, Vol. 14(2S) 163S–172S.
-
Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J Mater Sci: Mater Med (2014) 25:2445–2461
-
Donor site morbidity following iliac crest bone harvesting for cervical fusion: a comparison between minimally invasive and open techniques. Raymond Pollock. Eur Spine J (2008) 17:845–852.
-
Sandor GKB, Rittenberg BN, Clokie CML et al (2003). Clinical success in harvesting autogenous bone using a minimally invasive trephine. J Oral Maxillofac Surg 61:164–168.
-
Bykowski et al., A Multimodal Preemptive Analgesic Protocol for Alveolar Bone Graft Surgery: Decreased Pain, Hospital Stay, and Health Care Costs. The Cleft Palate-Craniofacial Journal 1-8
-
Yeung et al., Anterior cervical discectomy and fusion for cervical myelopathy using stand-alone tricortical iliac crest autograft: Predictive factors for neurological and fusion outcomes. Journal of Orthopaedic Surgery 27(3) 1–9 (2019).
-
Haws BE, et al. Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL, USA Impact of Iliac Crest Bone Grafting on Postoperative Outcomes and Complication Rates Following Minimally Invasive Transforaminal Lumbar Interbody Fusion. Neurospine 2019;16(4):772-779.
-
Park JJ, Hershman SH, Kim YH. Updates in the use of bone grafts in the lumbar spine. Bull Hosp Jt Dis. 2013;71(1):39-48.
-
Benzel and Gilbertson Enhancing Spinal Fusion Clinical Neurosurgery • Volume 55, 2008.
-
A.H. Schmidt. Autologous bone graft: Is it still the gold standard? Injury 52S2 (2021) S18–S22 Published by Elsevier Ltd. Hennepin Healthcare, Dept. of Orthopaedic Surgery, mail code G2, 701 Park Ave. South Minneapolis, MN 55415, USA
-
Emily Jane Bone grafting repairs damaged bones with transplanted tissue. J ORTHOP TRAUMA SURG REL RES 19(4) 2024.
-
Reisener et al., Trends in lumbar spinal fusion. Journal of Spine Surgery, Vol 6, No 4 December 2020. J Spine Surg 2020;6(4):752-761
-
Zhang et al. Osteogenic Biomaterials for Interbody Fusion. Biomaterials for Interbody Fusion
-
Bone Tissue Engineering Frontiers in Bioengineering and Biotechnology | www.frontiersin.org May 2022 | Volume 10 | Article 900992
-
Agarwal and García. Biomaterial strategies for engineering implants for enhanced osseointegration and bone repair. Rachit Agarwal and Andrés J. García Woodruff School of Mechanical Engineering, Georgia Institute of Technology, Atlanta, GA, USA Petit Institute for Bioengineering and Bioscience, Georgia Institute of Technology, Atlanta, GA, USA Adv Drug Deliv Rev. Author manuscript; available in PMC 2016.
-
Schaaf et al., Donor site morbidity after bone harvesting from the anterior iliac crest. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:52- Department of Maxillofacial Surgery, University Hospital Giessen and Marburg GmbH, Giessen, Germany.
-
Ralph J Mobbs, MD, Mina Chung, MD, Prashanth J Rao, MD, Bone Graft Substitutes for Anterior Lumbar Interbody Fusion. Orthopaedic Surgery 2013;5:77–85. Orthopaedic Surgery Volume 5 · Number 2 · May, 2013.
-
Othman et al., Artificial disc replacement in spine surgery. Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, NY, USA. Ann Transl Med 2019;7(Suppl 5):S170
-
G H Shepard, W J Dierberg. Use of the cylinder osteotome for cancellous bone grafting. Plast Reconstr Surg. 1987 Jul;80(1):129-32.
-
JUSTIN F. FRASER, M.D., AND ROGER HÄRTL, M.D. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine 6:298–303, 2007
-
Archunan M W, Petronis S (September 04, 2021) Bone Grafts in Trauma and Orthopaedics . Cureus 13(9): e17705.
-
Andrzejowski and Giannoudis. The ‘diamond concept’ for long bone non‑union management. J Orthop Traumatol (2019) 20:21
-
Autologous Bone Grafting. Operative Techniques in Sports Medicine. Volume 28, Issue 4, December 2020, 150780 Patrick G Robinson MRCS, Geoffrey D. Abrams MD, Seth L. Sherman MD, Marc R. Safran MD, Iain R. Murray FRCS, PhD. Department of Trauma and Orthopaedic Surgery, The University of Edinburgh, UK., Department of Orthopaedic Surgery, Stanford University, Palo Alto, CA
-
Zhang et al. Reconstruction of iliac crest defect after autogenous harvest with bone cement and screws reduces donor site pain. BMC Musculoskeletal Disorders (2018) 19:237 Burton DC, Carlson BB, Johnson PL, Manna BJ, Riazi-Kermani M, Glattes RC, Jackson RS. Backfilling of iliac crest defects withhydroxyapatite-calcium triphosphate biphasic compound: a prospective, randomized computed tomography and patient-based analysis. Spine J. 2013;13(1):54–61
-
Joseph Richard Dusseldorp Ralph J. Mobbs. Iliac crest reconstruction to reduce donor-site morbidity: technical note. Eur Spine J (2009). Department of Neurosurgery, Prince of Wales Hospital, Barker St., Randwick, NSW 2031, Australia. e-mail: joeduss@hotmail.com
-
Nancy E. Epstein. Iliac crest autograft versus alternative constructs for anterior cervical spine surgery: Pros, cons, and costs. SNI: Spine 2012, Vol 3, Suppl 3 - A Supplement to Surgical Neurology International.
-
Spontaneous Posterior Iliac Crest Regeneration Enabling Second Bone Graft Harvest; A Case Report. Elias C. Papadopoulos, MD Patrick F. O’Leary, MD Ioannis P. Pappou, MD Federico P. Girardi, MD Hospital for Special Surgery 2009 HSS Jrnl (2009) 5: 114–116.
Get in Touch
Reach out to our team to learn more information about our innovative bone grafting solutions and how they can elevate your orthopedic care practices and to enhance spinal fusion successes.
Workshop 'hands-on' training on human cadaver model, or on synthetic bone, is highly recommended by Dr. Brian P. Kelly and this can also be specially arranged.
Complete the form below to schedule a consultation.
For your information
For your information, as like every surgical procedure there is a step-by-step sequence protocol to follow, and clinical guidelines.
To learn more about the use of this minimally invasive ICBG harvesting technique, details, procedure demonstrations, the range of applications, training product samples and enquiries about workshop training, please contact :
Dr. Brian P. Kelly Ph.D.,
Barrow Neurological Institute,
350 West Thomas Road, Phoenix,
AZ 85013, USA.
email: brian.kelly@commonspirit.org
https://www.barrowneuro.org/person/brian-kelly-phd/
Dr. Benjamin Lee B.D.S.,
The Royal London Hospital, London E1 2AD, U.K,
email: drbenxjs@gmail.com
Dr. Ting Ho Ph.D.
Dr Chang IC MSc
Mr. Ricky Au MSc,
Biomedical engineer
email: rickyau@spintecgear.com

We are dedicated to enhance the overall successes of spinal fusion and orthopedic surgeries, the aim is for the lowest risks of complications overall. We look forward to receiving all your enquiries and we are ready to respond to you very promptly.
